Tiny retinal implant helps people with macular degeneration read again
A wireless retinal implant and smart glasses restored reading vision to people with macular degeneration, new research shows.
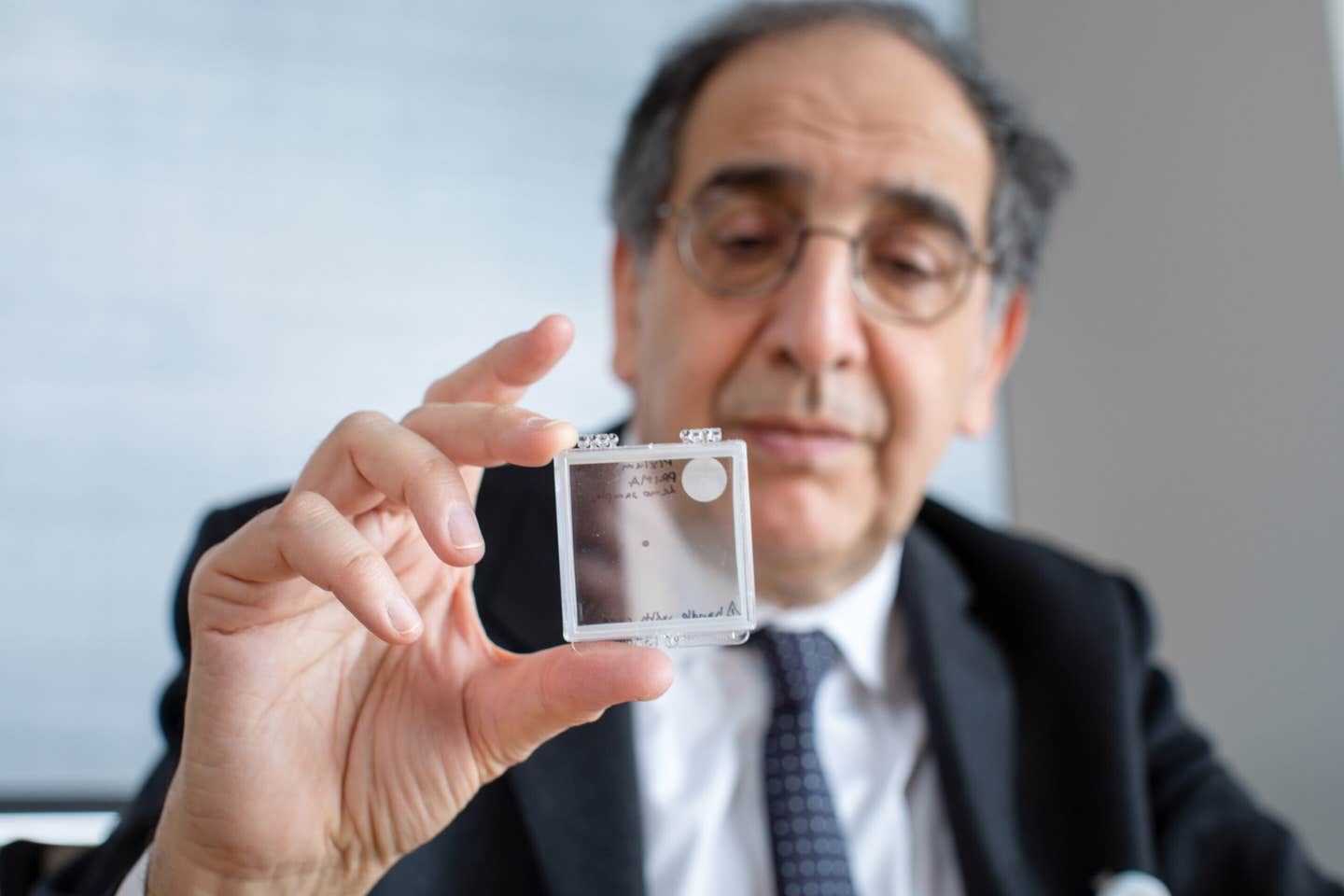
José-Alain Sahel, M.D., holding the PRIMA implant. (CREDIT: UPMC)
A small wireless chip and a pair of smart glasses are offering new hope to people who thought they’d never read again. The groundbreaking device, called PRIMA, has partially restored vision in people with advanced age-related macular degeneration — a condition that robs more than 5 million people worldwide of their central sight.
Developed by researchers at Stanford Medicine and tested across 17 hospitals in Europe, the PRIMA system uses light and electricity to replace the work of damaged eye cells. After one year of use, most participants in a major international trial could once again make out letters, words, and even full lines of text.
“It’s the first time that any attempt at vision restoration has achieved such results in a large number of patients,” said Dr. José-Alain Sahel, chair of ophthalmology at the University of Pittsburgh School of Medicine. “More than 80% of the patients were able to read letters and words, and some of them are reading pages in a book.”
How the PRIMA Device Works
The PRIMA system combines a miniature photovoltaic implant and a pair of glasses equipped with a built-in camera. The glasses capture the surrounding scene, then project the images using invisible near-infrared light onto the implant — a chip about 2 millimeters wide and thinner than a human hair.
The chip sits under the retina in the area where light-sensitive photoreceptors have died. It converts the projected infrared light into electrical signals, stimulating the remaining healthy retinal neurons and sending information to the brain. Patients use their natural peripheral vision alongside the prosthetic central vision, giving them a combined field of view that helps with orientation and movement.
Dr. Daniel Palanker, a Stanford ophthalmology professor who co-led the trial, said the design takes advantage of the eye’s transparency and natural wiring. “All previous attempts to provide vision with prosthetic devices resulted in basically light sensitivity, not really form vision,” he said. “We are the first to provide form vision.”
Because the implant is photovoltaic — generating current from light — it works wirelessly. Earlier devices required power cables exiting the eye, but PRIMA runs entirely on light projected from the glasses.
From Darkness to Reading Again
The international PRIMAvera clinical trial involved 38 participants, all over 60 years old, who had a severe form of macular degeneration called geographic atrophy. This condition gradually erodes central vision, making it impossible to read or recognize faces while leaving peripheral sight intact.
Each participant had worse than 20/320 vision in at least one eye before the surgery. After implantation, patients waited several weeks for healing before activating the chip and beginning vision training.
Learning to use the device wasn’t instant. “It may take several months of training to reach top performance,” Palanker said, comparing it to how patients with cochlear implants need time to interpret new sound signals. But as they practiced, progress was remarkable.
After a year, 26 of the 32 participants who completed the trial showed a clinically meaningful improvement in visual acuity — at least two additional lines on a standard eye chart. On average, their vision improved by about five lines, with one patient improving by 12. Twenty-seven participants reported being able to read with prosthetic vision, while others used the system to navigate or recognize signs.
Two-thirds of participants reported moderate to high satisfaction with their vision gains. Using the glasses’ digital tools, such as zoom and contrast adjustments, some achieved reading ability close to 20/42 vision.
A Patient’s Experience
For many, the impact went far beyond numbers on a chart. Sheila Irvine, one of the patients treated at Moorfields Eye Hospital in London, said she had lived with black patches in her vision before the procedure.
“I was an avid bookworm, and I wanted that back,” she said. “It’s a new way of looking through your eyes, and it was dead exciting when I began seeing a letter. It’s not simple, learning to read again, but the more hours I put in, the more I pick up.”
She now challenges herself by reading tiny labels, doing crosswords, and even checking her prescriptions — things that once seemed impossible. “It’s made a big difference,” she said. “Reading takes you into another world. I’m definitely more optimistic now.”
Mr. Mahi Muqit, associate professor in the UCL Institute of Ophthalmology and senior vitreoretinal consultant at Moorfields Eye Hospital, said the results mark a turning point in artificial vision. “Blind patients are actually able to have meaningful central vision restoration, which has never been done before,” he said. “Getting back the ability to read is a major improvement in their quality of life, lifts their mood and helps restore confidence and independence.”
The implantation itself takes under two hours and can be performed by any trained retinal surgeon. The device is activated about a month later, when the eye has fully healed. Artificial intelligence software in the glasses helps process the video feed, allowing the patient to focus and zoom in on text or objects.
Looking Ahead
In total, 19 participants in the study experienced temporary side effects, such as eye pressure or small retinal tears, but nearly all resolved within two months. Importantly, none lost any of their remaining peripheral vision.
While PRIMA currently delivers only black-and-white vision, the team is developing software to restore grayscale and, eventually, color. Future versions will also feature much smaller pixels — from 100 microns today to 20 microns — which could give patients up to 20/80 vision. With digital zoom, they might even approach 20/20 sight.
Researchers hope the technology could eventually be adapted for other causes of blindness that destroy photoreceptors. “This is the first version of the chip, and resolution is relatively low,” Palanker said. “The next generation will have better resolution and sleeker glasses.”
The trial’s strong results have led Science Corporation, the company developing PRIMA, to seek approval for clinical use in Europe and the United States. If authorized, it could become the first medical device to restore functional central vision in people with advanced macular degeneration — a milestone decades in the making.
Practical Implications of the Research
The success of the PRIMA implant marks a new era for treating irreversible blindness. It shows that sight lost to retinal degeneration can be partially restored, offering independence and hope to millions affected by geographic atrophy and similar conditions.
As next-generation implants deliver higher resolution and grayscale vision, the technology could help people not only read again but also recognize faces, navigate complex environments, and regain a sense of normalcy. The approach may even pave the way for future brain-computer interfaces that communicate visual information directly to the brain, extending the frontiers of neuroengineering and sensory restoration.
Research findings are available online in The New England Journal of Medicine.
Related Stories
- Breakthrough eye drops reverse vision loss from age-related macular degeneration
- New mRNA vaccine shows promise for preventing blindness
- New AI tool can predict the risk of severe vision loss
Like these kind of feel good stories? Get The Brighter Side of News' newsletter.
Joshua Shavit
Writer and Editor
Joshua Shavit is a Nor Cal-based science and technology writer with a passion for exploring the breakthroughs shaping the future. As a co-founder of The Brighter Side of News, he focuses on positive and transformative advancements in technology, physics, engineering, robotics and astronomy. Joshua's work highlights the innovators behind the ideas, bringing readers closer to the people driving progress.



