UCLA develops new immune cell therapy to battle deadly kidney cancer
UCLA’s new off-the-shelf cell therapy shows promise against hard-to-treat kidney cancer, bypassing the need for patient-specific treatments.

UCLA scientists created AlloCAR70-NKT, a ready-to-use immune cell therapy that targets kidney cancer from multiple angles—without customizing for each patient. (CREDIT: Shutterstock)
Researchers at UCLA have developed a powerful new weapon in the battle against kidney cancer. Instead of relying on treatments tailored to each patient, this innovation uses specially engineered immune cells that can be given to anyone. Known as AlloCAR70-NKT, this therapy works off-the-shelf—ready to use without customization.
This is a big step forward. Many current cancer treatments are time-consuming, expensive, and personalized. Patients often wait weeks to receive cells engineered from their own blood. In contrast, AlloCAR70-NKT skips that step. These lab-made cells come from stem cells and are pre-equipped with cancer-fighting tools.
“We successfully turned stem cells into powerful cancer-fighting immune cells that can be ready to use for any patient,” said Dr. Lily Wu, a professor at UCLA’s David Geffen School of Medicine. “This approach overcomes the time delays and safety risks of traditional immunotherapies, especially for patients with aggressive, late-stage disease.”
The new therapy could bring real change. It might improve survival, reduce harmful side effects, and help more people get treated—especially those running out of options.
Why Kidney Cancer Needs Better Solutions
Metastatic renal cell carcinoma, or advanced kidney cancer, is hard to treat. While new immunotherapy drugs have helped some people, many patients don’t respond. Others get better at first, only to see the cancer return. Right now, the five-year survival rate for this aggressive disease is just 12%.
This kind of cancer often resists traditional treatments. It creates a tough environment in the body that shields it from attacks. For doctors and scientists, this makes it harder to develop lasting cures.
Knowing this, researchers at UCLA’s Jonsson Comprehensive Cancer Center and the Broad Stem Cell Research Center decided to try something different. They built a new therapy designed to outsmart the tumor and its defenses, using the body’s own immune tools in a smarter way.
Related Stories
- Cambridge scientists reprogram brain cancer cells to stop them from spreading
- Combination of three immune-targeting drugs offers new hope for skin cancer patients
Engineering the Perfect Fighter Cells
The science behind AlloCAR70-NKT is both cutting-edge and practical. The researchers started with stem cells. These are special cells that can grow into almost any type of cell in the body. From these, they built immune cells called NKT cells—short for natural killer T cells.
NKT cells are known for their strong immune abilities. But these weren’t ordinary cells. The team gave them a new weapon: a chimeric antigen receptor, or CAR, designed to target a protein called CD70. This protein is commonly found on the surface of kidney cancer cells. By adding the CAR, the researchers helped the cells “see” and attack tumors more easily.
“We tackled a challenge in cancer immunotherapy,” said Dr. Lili Yang, another senior researcher on the study. “Our goal was to create an off-the-shelf therapy that persists and works in patients without causing serious immune complications.”
Many existing CAR-T therapies work well in blood cancers but struggle with solid tumors like kidney cancer. Tumors in organs often block immune cells from entering. Even when cells get in, the cancer’s environment can shut them down.
To solve that, UCLA’s scientists gave their NKT cells three main strengths. First, they equipped them to kill cancer cells directly—using both the new CAR and their natural NKT receptors. This helped even when the cancer had low levels of CD70, which normally makes it harder to treat.
Second, they taught the cells to weaken the tumor’s surroundings. Cancer often builds a protective wall made of immune-suppressing cells. AlloCAR70-NKT breaks that down, making it easier for immune cells to move in and attack.
Third, they designed the therapy to remove certain host immune cells that would normally fight off the donor cells. This lets the therapy last longer in the body. At the same time, the cells don’t stay forever, so they’re less likely to cause long-term problems like immune system damage.
“This multi-pronged approach helps them attack both the tumor and its surrounding support system,” said Dr. Arnold Chin, a urology professor and co-senior author of the study. “It makes them a potent, multifunctional and safer option for metastatic kidney cancer.”
The Power of Preclinical Results
In lab studies using models of kidney cancer, the results were striking. The engineered cells showed strong anti-cancer activity on several levels.
First, they killed cancer cells directly. Even tumors that didn’t have much CD70 were attacked. That matters, because many treatments lose power when a tumor has low amounts of the target protein.
Second, the cells worked inside the tumor’s microenvironment. Normally, this area protects the cancer. But the engineered NKT cells didn’t just survive there—they actively reprogrammed it. That allowed other immune responses to kick in, reinforcing the attack.
Third, by clearing out CD70-positive host immune cells, the therapy lowered the chance of being rejected by the body. This gives the therapy more time to work. And since the cells naturally fade away over time, the risk of long-term harm drops, too.
All these effects combined into a powerful treatment. In preclinical testing, the tumors shrank significantly. While the research hasn’t moved into large human trials yet, the early success offers strong hope.
“If the early promise translates to patients, it could offer a new lifeline for many,” said Chin.
What Comes Next?
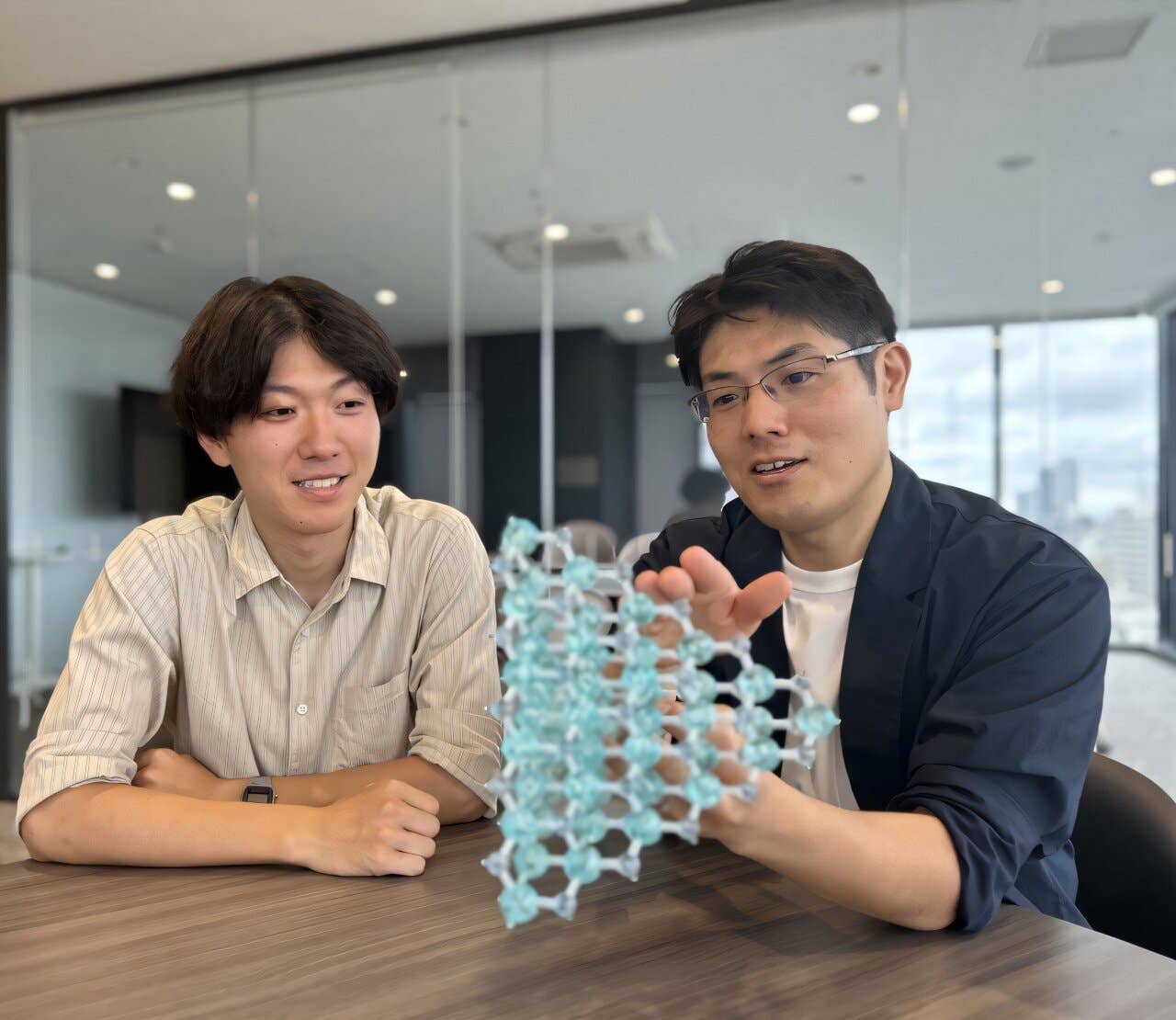
The study, published in Cell Reports Medicine, was led by first authors Yan-Ruide Li and Junhui Hu, both scientists at UCLA. The full team includes members from multiple departments, showing the collaborative effort behind the discovery.
The work was supported by grants from the California Institute for Regenerative Medicine, the Parker Institute for Cancer Immunotherapy, and the U.S. Department of Defense’s Kidney Cancer Research Program.
Because this therapy doesn’t rely on cells from each individual patient, it could eventually be manufactured at scale. That could make it more affordable and more accessible, especially for clinics that don’t have the resources for complex cell engineering.
Yang, Wu, and Chin—all key figures on the project—are also members of multiple research centers at UCLA, including the Microbiome Center and the regenerative medicine program. Their work highlights how university research can directly lead to next-generation treatments.
Many questions remain. Human trials are needed to confirm the safety and effectiveness of AlloCAR70-NKT. Researchers must also learn how long the cells last in real patients, how best to deliver them, and how they interact with other therapies.
Still, the study marks a major step forward. For people with metastatic kidney cancer—especially those who have tried other options without success—this kind of therapy could open the door to better outcomes.
By building smarter immune cells and designing them to act fast, last longer, and avoid rejection, UCLA’s team may have set the stage for a new era in cancer treatment.
Note: The article above provided above by The Brighter Side of News.
Like these kind of feel good stories? Get The Brighter Side of News' newsletter.