Scientists edit mitochondrial DNA to reverse genetic diseases which often have no cure
Scientists have used a base editor to fix mutations in mitochondrial DNA, paving the way for new treatments for genetic diseases.
New study shows base editors can fix mitochondrial DNA mutations, opening doors to treat rare genetic diseases. (CREDIT: CC BY-SA 4.0)
For decades, the dream of fixing harmful mutations in mitochondrial DNA felt out of reach. Scientists have long known these mutations cause serious diseases that pass down only through mothers. They also play a role in cancer and many conditions related to aging. But unlike normal DNA in the cell nucleus, mitochondrial DNA sits behind a protective barrier. Standard genetic editing tools like CRISPR cannot reach it.
Now, researchers from the Netherlands have shown a way forward. In a study published in PLOS Biology, the team used a tool called a base editor to fix single-letter mutations in mitochondrial DNA without cutting it. This work could lead to treatments for people living with mitochondrial diseases, which often have no cure.
Why Mitochondrial Mutations Matter
Mitochondria are tiny compartments inside your cells. They create the energy that powers almost every process in the body, from thinking to moving to healing. Each mitochondrion carries its own small set of DNA, passed only through mothers. If there is a mistake in this DNA, it can cause problems throughout the body.
Some mutations lead to severe disorders that appear in childhood, affecting muscles, the brain, and the heart. Others damage cells slowly over time, contributing to diseases like cancer or age-related decline.
For years, scientists used CRISPR to edit nuclear DNA. CRISPR works like molecular scissors, cutting out faulty parts so cells can repair themselves. But CRISPR cannot cross the double membranes of mitochondria. This left patients with mitochondrial diseases behind in the gene editing revolution.
The Power of Base Editors
In this new study, the Dutch team turned to a tool called a double-stranded DNA deaminase toxin A-derived cytosine base editor, or DdCBE. Unlike CRISPR, DdCBE does not cut DNA. Instead, it changes a single letter – for example, switching a C to a T – without breaking the strand.
Related Stories
DdCBE combines parts of a bacterial toxin with proteins called Transcription Activator-Like Effectors, or TALEs, that guide the tool to the exact spot in the DNA. This precision reduces the risk of unwanted edits.
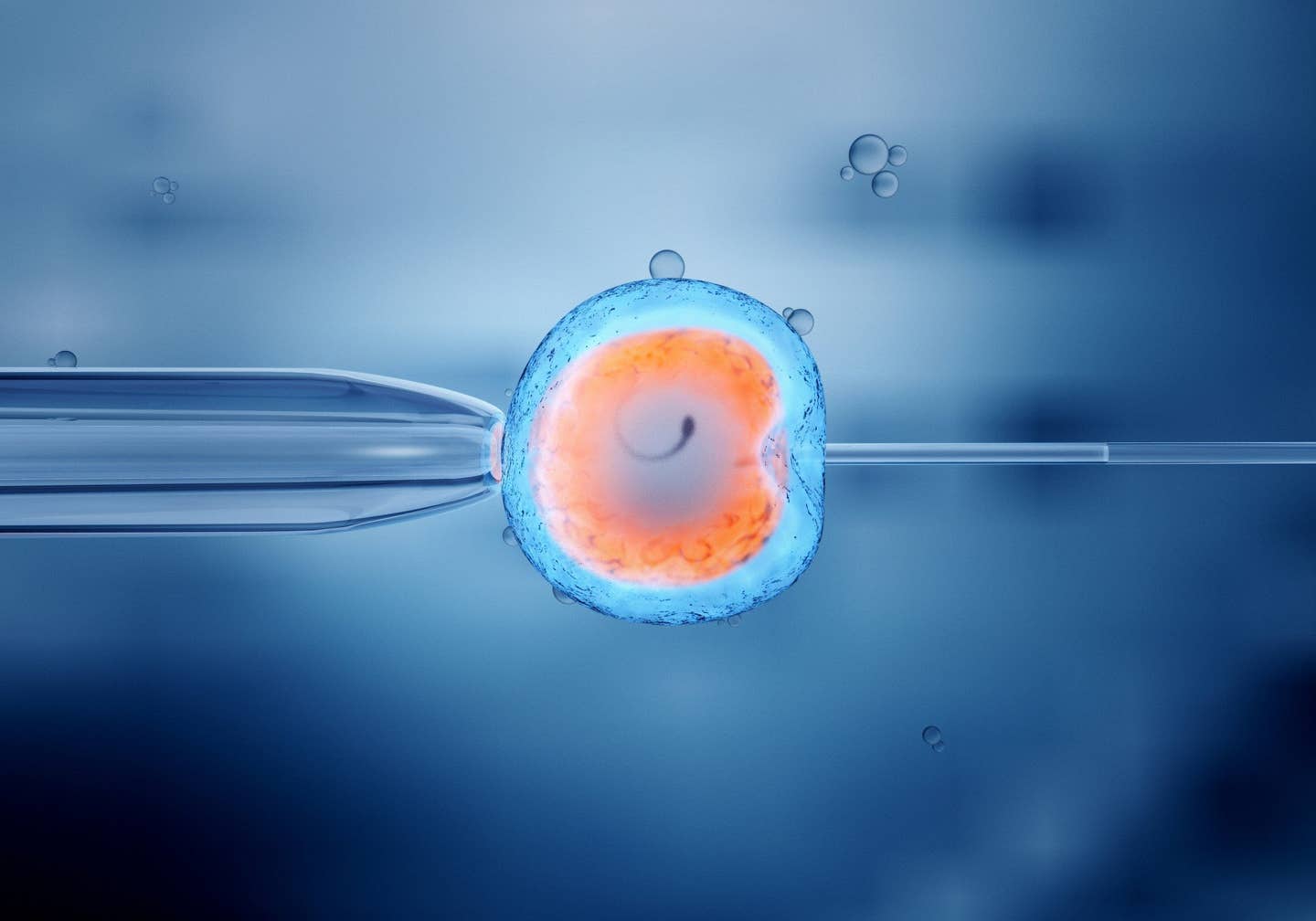
Researchers tested DdCBE on cells from two types of tissues linked to mitochondrial diseases. First, they engineered liver cells to carry a harmful mutation. This mutation impaired the cell's ability to produce energy. Then they used DdCBE to introduce the mutation into human liver organoids – tiny, lab-grown versions of the liver.
The editing worked. In organoids carrying the mutation, energy production dropped by 23 percent. This showed that their engineered disease model could mimic what happens in real patients. The researchers also noted that editing efficiency varied across individual cells, from no edits to up to 80 percent edited DNA. This variability could help study how different levels of mutation affect disease severity.
Correcting Patient-Derived Skin Cells
Next, the team focused on fixing a different mutation. They worked with skin cells taken from a patient with Gitelman-like syndrome, a mitochondrial disorder. These cells carried a mutation in the gene MT-TI, which codes for a molecule needed to build proteins inside mitochondria.
Using DdCBE, the researchers corrected the mutation in these fibroblast cells. After editing, the cells showed restored mitochondrial membrane potential – a sign that the mitochondria were working properly again. Clonal analysis revealed that edited cell lines maintained or even increased the proportion of corrected DNA over 50 days. This suggests the correction does not harm the cells or make them less competitive.
How Delivery Methods Matter
One hurdle in gene editing is how to get the editing tool into the cell safely. Traditional methods use DNA plasmids, which can be toxic and trigger immune reactions. In this study, the team tested two advanced delivery methods: sending the editor as mRNA or packaging it within lipid nanoparticles.
Delivering the editor as mRNA increased editing efficiency and kept cells healthier compared to DNA delivery. Lipid nanoparticles, tiny fat bubbles that carry genetic material into cells, also worked well. This method is already used in vaccines, such as those for COVID-19, and is considered one of the safest delivery systems.
Importantly, the edits were specific. Few off-target edits appeared in the nuclear DNA, and only a small number occurred elsewhere in mitochondrial DNA. This precision reduces the risk of accidental damage that could lead to cancer or other complications.
A Leap for Mitochondrial Medicine
For people with mitochondrial diseases, these findings bring hope. Current treatments only manage symptoms. There is no cure for most mitochondrial disorders because their root cause lies in hard-to-reach DNA. With base editing, doctors could one day fix these errors at the source.
“The potential of mitochondrial base editing in disease modeling and potential therapeutic interventions makes it a promising avenue for future research and development in mitochondrial medicine,” the authors wrote.
They added, “Mitochondrial patients have not been able to benefit from the CRISPR revolution for so long, but recently the technology has come available with which we can finally repair mitochondrial mutations.”
Challenges Ahead
Despite this progress, challenges remain. Base editing has only been tested in the lab so far. It will take years of animal studies and clinical trials to prove it is safe and effective in humans. Researchers must also find ways to edit enough mitochondria in each cell to reverse disease symptoms without harming healthy tissue.
Another issue is the variation in editing efficiency between cells. Some cells show high correction levels while others show little change. Scientists need to understand what causes this difference to ensure treatments work reliably.
The possibility of off-target edits, though low, must also be explored. Even a single unintended edit in the wrong place could have serious effects. However, the current study used advanced forms of DdCBE designed to minimize such risks.
Moving Toward Clinical Application
The research team prepared for future clinical use by testing the editing tool in ways similar to potential patient treatments. Using lipid nanoparticles and mRNA is a step toward therapies that do not rely on viruses or risky DNA delivery methods.
They introduced the m.15150G > A mutation in liver organoids to create models with varying degrees of heteroplasmy – the mix of mutated and normal mitochondrial DNA. Cells with about 24 percent mutated DNA showed reduced energy production, confirming the model's validity for studying disease mechanisms.
In skin fibroblasts, the correction of the m.4291T > C mutation improved mitochondrial function without reducing cell health over long-term culture. This suggests that corrected mitochondria can persist and function well, an important factor for durable treatments.
The Future of Mitochondrial Editing
This breakthrough adds to a growing list of base editing successes. Earlier studies showed DdCBE could create mitochondrial disease models in animals like zebrafish and rodents. Scientists have also edited human embryos and developed adenosine base editors to change different DNA letters.
But this study stands out. It demonstrates both the creation of disease models and the correction of patient-derived cells using methods that could translate into real therapies.
The work, conducted at the University of the Netherlands, shows how far mitochondrial genetics has come. Once left behind by CRISPR, the field is now catching up. The combination of precision editing tools with safe delivery methods could finally bring cures for disorders long considered untreatable.
For now, these results remain in the lab. But each discovery builds toward a future where people born with mitochondrial mutations can live healthier lives.
Note: The article above provided above by The Brighter Side of News.
Like these kind of feel good stories? Get The Brighter Side of News' newsletter.